When you’re prone to acne, you often experience scarring too. It’s a normal part of the healing process but, just like the acne itself, the pigmentation and uneven skin texture left behind can have an impact on your self-esteem. The good news is, it’s treatable. Here’s everything you need to know about acne marks and what you can do about them.
Types of Acne Marks
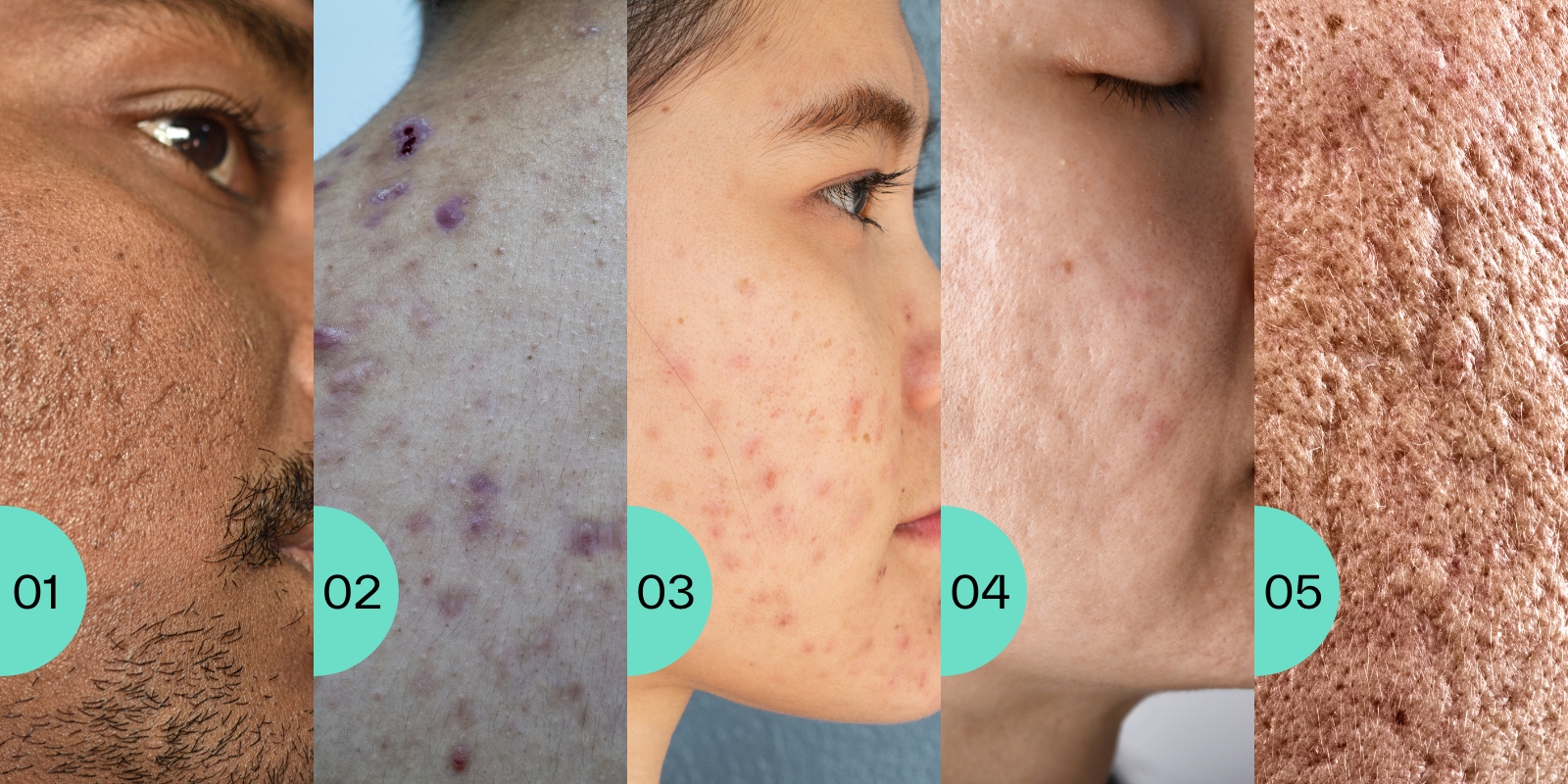
To explore the different kinds of acne marks, first it’s important to know what they look like and why they happen.
Peri and post-inflammatory hyperpigmentation
When people refer to ‘acne marks’ or ‘dark marks’, this is usually what they’re talking about.
Peri and post-inflammatory hyperpigmentation (PIH) are caused by an inflammatory response in the skin, which often happens with conditions like acne. Inflammation is part of your skin’s healing process, but melanin-producing cells are part of this immune response. They’re activated when your skin gets inflamed, which can make them produce excess pigment. These types of hyperpigmentation are very similar, but happen at slightly different stages:
Peri-inflammatory hyperpigmentation means the pigmentation appears at the same time as your active acne.
Post-inflammatory hyperpigmentation means the inflammation caused when your acne has gone away, but the pigment is still visible.
It’s important that before treating pigmentation, we treat your active acne first. This is because the longer the condition goes on, the more pigment is produced. PIH can happen with any skin type, but it’s more common in brown and black skin (Fitzpatrick skin types 4–6). Around 60% of people with black skin will have PIH after acne, and it’ll generally be purple or brown in colour with this skin type. It can take 6–12 months to clear on its own, but in 20% of cases, it can take even longer — even up to 5 years. It all depends on the depth of the hyperpigmentation and areas affected. However, it can clear quicker with the help of powerful ingredients like topical retinoids, azelaic acid and hydroquinone, once you know which one to use.
Post-inflammatory hypopigmentation
When your skin’s melanin-producing cells respond to inflammation, they don’t always create excess pigment. Sometimes they react by producing the normal amount of melanin. Or, sometimes they even decrease their melanin production. In these cases, you get post-inflammatory hypopigmentation. This is where the melanin-producing cells reduce the amount of pigment they create, resulting in lighter patches on the skin where your inflammation was. You don’t usually need to do anything about hypopigmentation once you’ve started using actives to treat your acne, but a GP or Dermatology specialist can prescribe specific medicines if you haven’t seen an improvement over time.
Post-inflammatory erythema
Post-inflammatory erythema (PIE) happens when your blood flow increases while an area of acne on your skin is inflamed. This can cause your blood vessels to widen or become damaged, leaving red or pink marks on the skin. Blood vessel damage might sound serious, but PIE is normal and usually settles on its own in a few weeks. It’s more common in white skin, but can still occur in all skin types.
Acne scarring
Like post-inflammatory hyperpigmentation, acne scarring happens as part of your skin’s healing process in breakout-prone areas. This usually happens in moderate to severe cases of acne, but it can happen with milder flare-ups, too — it’s most common where nodules or cysts have been on the skin.
Acne scarring forms during the natural wound healing process, where skin cells produce collagen and a protein called keratin to help repair the area affected by a spot. The amount and type of scarring you get depends on several factors, like genetics and the severity of your acne. Here are some examples of how acne scarring can appear:
Ice-pick scars: small, deep, narrow, pitted scars.
Rolling scars: broad scars with sloping edges.
Boxcar scars: broad scars with sharp borders.
Hypertrophic or keloid scars: thick scars, raised above the skin surface.
We know that it can be frustrating to experience scarring so soon after healing your acne. It’s important to remember though, it’s all part of your skin’s natural healing process and is easily treatable after your breakouts and pigmentation have cleared.

How does Dermatica treat acne marks?
Now we know more about the different types of acne marks, how do you treat them? This will depend on whether you still have active acne, and the type of acne mark you’re experiencing. Here are some of the steps we, or your dermatologist, can take:
I currently have acne, I’d like to treat hyperpigmentation and/or scarring
If you still have active acne, our first priority is to treat and clear your breakouts. This is because there’s always a chance of more hyperpigmentation forming as they heal. Stopping breakouts will also help reduce the risk of any scars developing. A topical formula containing retinoids like adapalene or tretinoin will help treat your acne by reducing inflammation and unclogging pores, while other ingredients like benzoyl peroxide help keep acne-causing bacteria at bay.
To learn more about the best ingredients for treating acne, check out our blog post. The great news about our ingredients is that they’re often multi-tasking — so we use them to treat hyperpigmentation, too. While your acne is clearing, your formula will also work to fade any dark marks your spots leave behind. Then once you’re ready, our dermatology experts will transition you onto a skincare formula that’s clinically proven to fade hyperpigmentation after the acne has cleared.
Both of these treatment plans will help to improve the texture of your skin, which could help with mild scarring, too. Any deep or hypertrophic scars unfortunately won’t respond to a topical formula alone, so will most likely need a specialist.
My acne has cleared, but I have scarring and hyperpigmentation
Once your breakouts have been treated, our dermatology experts will recommend a formula that contains pigment-fading actives like hydroquinone and azelaic acid. While using this formula, it’s really important to apply daily sun protection (a broad-spectrum sunscreen, at least SPF 30) and avoid direct sunlight in summer months. This is because UV exposure can worsen hyperpigmentation by making it darker and harder to fade.
To learn more about treating hyperpigmentation, check out our blog.
My acne and hyperpigmentation have improved — I’d like to treat my scarring
Topical retinoids like adapalene and tretinoin may help improve mild to moderate acne scarring. Try using a retinoid formula for around 12 weeks to see if it helps. Although our treatments can help improve your skin’s overall texture, more severe, raised scarring like hypertrophic or keloid scars often need the help of a specialist. Dermatology clinics can provide you with a face-to-face consultation and acne scar treatment plan, which can include techniques like chemical peels, dermabrasion and laser treatments. Again, to make sure you can get the best results — and prevent any harmful side effects — it’s really important that all active acne is cleared before you look into these scar treatments.
Need help treating acne, hyperpigmentation or another skin condition? Complete your free online consultation today and our clinical experts will recommend a personalised formula suited to your skin goals.
Dr Catriona Maybury
Dr Catriona Maybury is a Consultant Dermatologist, working as Medical Lead for Dermatica and at St George’s Hospital in London. Catriona completed her specialty training at St John’s Institute of Dermatology in London. Catriona has a special interest in medical dermatology, completing a PhD in liver fibrosis amongst psoriasis patients at King’s College London. Catriona is a certified coach and worked as Dermatology Section Editor for the British Medical Journal.